Earlier this summer, Aaryn and I reached out to the greater allergy community and asked "what are the fears, myths, or questions you have/have heard about OIT?". Foolishly, I posted this question before heading to bed, thinking we would get a few questions. The next morning, I woke up to several dozen notifications. When all was said and done, we had over 50 questions! That list was reviewed, and 20 questions remained (for those wondering about the other questions, some were combined, others will be saved for a less fact-focused, more experience centered article). We reached out to none other than the renowned (and much loved) Dr. Richard Wasserman of The Dallas Food Allergy Center. We are thrilled that he agreed to answer our (fairly long) list of questions!
PART ONE: The Basics
OrAAA: What does your protocol look like? What is the ultimate goal?
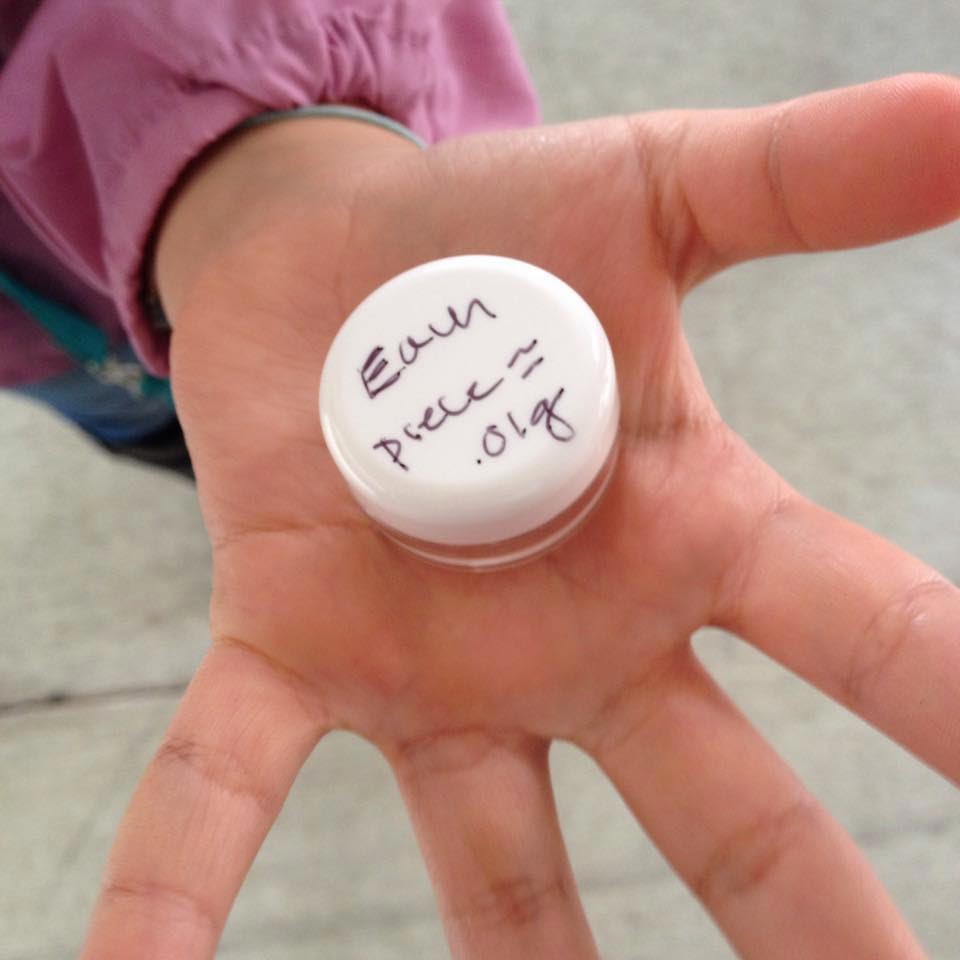
Dr. Wasserman: We
begin with a very low dose, no patient has ever reacted to our first
dose. On day one we give several doses over a several hour period. After
the first day, we do dose increases weekly. The target dose is a full
portion of the food. Our goal is normal life. For most patients, the
goal is to freely incorporate the food into their diet. Not all patients
are able to do that. Some families decide that they want to continue to
avoid the problem food even after they complete OIT.
Dr: Wasserman: OIT, sublingual and the patch all work on the principles of desensitization that introduce progressively increasing doses of allergen over time to alter the allergic response. This approach has been used by allergists for more than 100 years. The mechanism of action of FAHF-2 is still being worked out.
Dr. Wasserman: Whenever a
patient begins OIT, there will always be a question of whether the
symptom was caused by the OIT food. Therefore, other allergy related
problems need to be well controlled before OIT is started. This applies
to allergies, asthma and eczema. We have no experience with OIT in
patients with mast cell activation syndrome or idiopathic anaphylaxis
and would be reluctant to try in those cases because it would be hard to
differentiate a food reaction from other problems. The understanding of
EoE and FPIES is limited and the risks of introducing a food known to
cause a reaction are unknown but those problems are difficult enough
without adding the potential complications of OIT. We would not begin
OIT in a patient with EoE or FPIES.
Dr. Wasserman: We
believe that about 3-5% of our OIT patients develop clinical symptoms
suggestive of EoE. Some groups have seen a higher incidence. Early on,
when these symptoms occurred (vomiting hours after the OIT dose), we
stopped OIT. Based on the work of our colleague, Dr. Katz in Israel, we
now reduce the dose until symptoms resolve, hold at the lower dose for
several months, and then increase again. This works for most patients.
Food/exercise
anaphylaxis has been known for many years. Exercise too soon after
doing is a significant risk for a reaction. We require a two hour
waiting period after dosing before athletic activity.
OrAAA: There
seems to be a lot of different protocols out there (rest periods, bite
proof vs. unlimited consumption, once or twice a day, etc.). Do you
know why this is?
Dr. Wasserman: Each
allergist develops the approach that he or she believes will work the
best. Each OIT study can only tell us how well that protocol seems to
work. The only way to know if one is better than another would be to do a
study comparing them in a controlled fashion. It is unlikely that such a
study will ever be done. The protocol that we use today has been
modified several times based on review of our experience. We collected
detailed information about the experience of each OIT patient and review
that information at least annually. Based on what we see in the
compiled data we modify our approach to make it safer or better
tolerated. Among those who have reported their experience, the results
are pretty much the same.
OrAAA: Bite proof or unlimited...which is the better goal?
Dr. Wasserman: It
depends on the individual patient. We aim for unlimited incorporation
of the food into the diet. Very few children are so difficult to treat
that they can't reach the target dose but it does happen. So children
really hate the taste of the food, especially peanut. For those children
it doesn't really make sense to push to the full dose. The right goal
is the goal that is right for the individual child and family.
Dr. Wasserman: We really don't know. It appears that some children develop sustained unresponsiveness with profound reductions (>98%) of the food specific IgE. These children don't have to dose daily. At this point, it seems that most OIT patient will need to dose indefinitely. The allergic response is still only partially understood. We don't know why some people develop food allergy nor why some respond to OIT better than other.
Dr. Wasserman: There
is a lot of misunderstanding of the role of the FDA in OIT, even by
doctors. The FDA approves drugs and devices. It never approves
treatments. It is likely that the FDA will eventually approve the peanut
treatment being developed by Aimmune. I see this as a disaster for
patients. I can treat many patients for a $6 bag of peanut flour. When
the FDA approves peanut treatment, I expect that the peanut drug will
cost thousands of dollars per patient excluding physician's fees.
OrAAA: Is there a chance that OIT can make an allergy WORSE?
Dr. Wasserman: I don't think that OIT can make an allergy worse.
OrAAA: There
seems to be pretty good consensus that adolescents are at risk for poor
outcomes associated with anaphylaxis. Is this biological or related to
another factor? If it is biological, does that mean that it could make
OIT dangerous at this age?
Dr. Wasserman: It
is hard to know for sure but I think the problem with adolescents is
that they deny early symptoms and don't carry epinephrine and therefore
treatment is delayed. We do know that delay in the use of epinephrine is
associated with bad outcomes.
Dr. Wasserman: Children
receiving OIT need to be developmentally able to fully cooperate with
the process, communicate subtle symptoms and be willing to eat a food
every day as though it was a medicine. Each child should be evaluated
individually before start OIT.
OrAAA: If OIT in the private practice is safe, why is it so controversial? Why the lack of practices?
Dr. Wasserman: It
has been argued publicly that more studies are needed before OIT can be
offered by allergists outside of studies. Since that statement was made
in a public forum, there have been more than 400,000 ER visits for food
allergy and opponents say we still need to wait for more studies. OIT
is a complex and demanding procedure for patients, their allergists and
their allergists' office staffs. Not every office will be equipped or
willing to undertake the effort to offer this therapy. I believe that
OIT should be available but I don't believe that every allergist should
offer OIT.
Dr. Wasserman is Medical Director of Pediatric Allergy and Immunology at Medical City Children’s Hospital and managing partner of Allergy Partners of North Texas. He served on the full time and clinical faculty in the Department of Pediatrics at the University of Texas Southwestern Medical School from 1988 to 2015.
He was raised in New York, where he graduated cum laude with Honors in Chemistry from Hobart College. He studied at Mt. Sinai School of Medicine and City University of New York Graduate School receiving his PhD in immunology from CUNY and his MD from Southwestern Medical School. He did an internship and residency in pediatrics and a fellowship in bone marrow transplantation and immunology at The Children’s Hospital of Philadelphia. After a fellowship at The Rockefeller University (Kunkel Lab) he became Chief of Pediatric Allergy and Immunology and Pediatric Program Director at Southwestern Medical School.
After six years as fulltime faculty, Wasserman started a private practice in allergy and immunodeficiency and DallasAllergyImmunology Research that has conducted more than 110 FDA approved studies. He served as Director of the Immunology Clinic at Children’s Medical Center of Dallas for 19 years and taught immunodeficiency to medical students for more than 25 years. He is a past president of the Pediatric Society of Greater Dallas and has edited the Society Newsletter for fifteen years. Wasserman is currently a Trustee of Hobart and William Smith Colleges and a past member of the AAAAI Board of Directors.
Wasserman has coauthored more than 100 peer-reviewed publications, case reports, book chapters and reviews and 80 International Meeting posters and presentations.
He was raised in New York, where he graduated cum laude with Honors in Chemistry from Hobart College. He studied at Mt. Sinai School of Medicine and City University of New York Graduate School receiving his PhD in immunology from CUNY and his MD from Southwestern Medical School. He did an internship and residency in pediatrics and a fellowship in bone marrow transplantation and immunology at The Children’s Hospital of Philadelphia. After a fellowship at The Rockefeller University (Kunkel Lab) he became Chief of Pediatric Allergy and Immunology and Pediatric Program Director at Southwestern Medical School.
After six years as fulltime faculty, Wasserman started a private practice in allergy and immunodeficiency and DallasAllergyImmunology Research that has conducted more than 110 FDA approved studies. He served as Director of the Immunology Clinic at Children’s Medical Center of Dallas for 19 years and taught immunodeficiency to medical students for more than 25 years. He is a past president of the Pediatric Society of Greater Dallas and has edited the Society Newsletter for fifteen years. Wasserman is currently a Trustee of Hobart and William Smith Colleges and a past member of the AAAAI Board of Directors.
Wasserman has coauthored more than 100 peer-reviewed publications, case reports, book chapters and reviews and 80 International Meeting posters and presentations.